Welcome to the first section of our article on effective obesity prevention strategies. In this section, I will introduce you to the different approaches and strategies that have shown promising results in combating obesity. Obesity is a major public health concern, and it requires comprehensive and targeted interventions to address its multifaceted causes.
Obesity prevention strategies focus on environmental and policy changes that can impact whole populations or high-risk subpopulations. These strategies aim to reverse the shift in the population distribution of BMI by lowering the mean BMI level and decreasing the incidence of obesity. Additionally, prevention for individuals who are already overweight or obese aims to avoid progression to a more severe level of obesity and prevent or delay the onset of obesity-related medical conditions.
There are three levels of obesity prevention interventions – universal, selective, and indicated – each targeting different population segments. Effective interventions often involve teachers acting as role models, school policies that support healthy food choices, changes in the school environment to increase physical activity, and active involvement of parents. By implementing these strategies, we can make significant progress in preventing and reducing obesity.
Key Takeaways:
- Obesity prevention strategies focus on population-based and multilevel approaches.
- Prevention efforts aim to lower the mean BMI level and decrease the incidence of obesity.
- Interventions can target different population segments through universal, selective, and indicated approaches.
- Effective strategies include involving teachers, implementing school policies, and engaging parents.
- Implementing these strategies can help prevent and reduce obesity in diverse settings.
Population Perspective on Obesity Prevention
https://www.youtube.com/watch?v=09SorG9DErE
From a population perspective, the goal of obesity prevention is to lower the mean body mass index (BMI) level and reduce the rate at which individuals enter the higher end of the BMI distribution. This can be achieved by stabilizing the BMI distribution or minimizing the incidence of new individuals crossing the relevant BMI threshold.
For adults who are at a healthy weight, prevention involves maintaining their current status and avoiding excess weight gain. On the other hand, for children, prevention focuses on maintaining a healthy weight trajectory and preventing excessive weight gain during their growth, development, and maturity.
For individuals who are already overweight or obese, prevention refers to avoiding the progression to a more severe level of obesity and/or preventing or delaying the onset of obesity-related medical conditions. It is essential to intervene early and address the underlying causes of obesity to effectively manage and prevent its consequences (check out my post on causes of obesity here).
The following table provides a visual representation of the BMI distribution and different weight categories from a population perspective:
| BMI Category | Health Risk |
|---|---|
| Underweight ( | Increased risk of malnutrition and related health issues |
| Normal weight (18.5-24.9) | Reduced risk of chronic diseases |
| Overweight (25-29.9) | Increased risk of developing chronic diseases |
| Obesity class I (30-34.9) | Moderate risk of developing obesity-related health problems |
| Obesity class II (35-39.9) | Severe risk of developing obesity-related health problems |
| Obesity class III (40 or higher) | Very high risk of developing obesity-related health problems |
Understanding the population perspective on obesity prevention is crucial for implementing effective strategies and interventions that address the diverse needs of different individuals and populations. By focusing on lowering the mean BMI level and reducing the incidence of obesity, we can make significant strides in preventing and managing this global health issue.
Types of Obesity Prevention

Obesity prevention can be categorized into three types: primary prevention, secondary prevention, and tertiary prevention.
- Primary prevention: This type of prevention aims to prevent the occurrence of obesity in the general population. It focuses on implementing interventions that target the entire population or high-risk subpopulations. The goal is to promote healthy behaviors and create environments that support healthy choices. By addressing the root causes of obesity, primary prevention strategies aim to reduce the overall prevalence of obesity in a population.
- Secondary prevention: Secondary prevention focuses on early detection and intervention to prevent the progression of obesity in individuals who are at risk. It aims to identify individuals who have a higher likelihood of developing obesity and provide targeted interventions to prevent or delay its onset. This may involve screening, counseling, and referral to specialized programs and services. By intervening at an early stage, secondary prevention strategies aim to prevent the worsening of obesity and its associated health consequences.
- Tertiary prevention: Tertiary prevention aims to prevent complications and manage the health consequences of obesity in individuals who are already obese. This type of prevention focuses on providing comprehensive care and support to help individuals manage their weight and prevent obesity-related complications, such as diabetes, heart disease, and joint problems. Tertiary prevention strategies may include medical treatment, lifestyle modifications, and ongoing support and monitoring.
By implementing a combination of primary, secondary, and tertiary prevention strategies, we can address obesity at different stages and target various population segments, ultimately reducing the burden of obesity and improving public health.
Summary:
In summary, obesity prevention can be classified into three types: primary prevention, which aims to prevent the occurrence of obesity in the general population; secondary prevention, which focuses on early detection and intervention in individuals at risk of obesity; and tertiary prevention, which aims to manage the health consequences of obesity in individuals who are already obese. By utilizing a comprehensive approach that incorporates all three types of prevention, we can effectively tackle the obesity epidemic and promote better health outcomes.
| Type | Definition |
|---|---|
| Primary prevention | Prevent the occurrence of obesity in the general population through interventions targeting the entire population or high-risk subpopulations. |
| Secondary prevention | Early detection and intervention to prevent the progression of obesity in individuals who are at risk. |
| Tertiary prevention | Prevent complications and manage the health consequences of obesity in individuals who are already obese. |
Image:
School-Based Obesity Prevention Programs
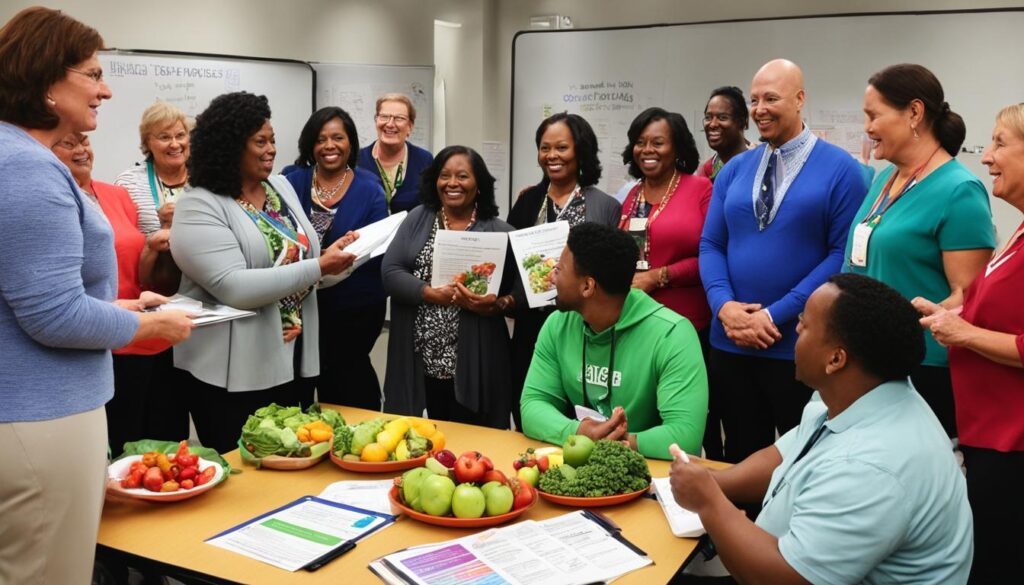
Elementary schools play a critical role in addressing childhood obesity through the implementation of prevention programs. These programs focus on promoting healthy eating habits, increasing physical activity, and reducing sedentary behavior among students (check this post out). By targeting children at a young age, these programs have the potential to instill lifelong healthy habits and prevent obesity-related health issues.
Studies have shown that school-based programs with multiple components yield the most significant improvements in obesity-related outcomes. By combining physical activity with nutrition education, these programs provide a comprehensive approach to promoting healthy behaviors. Additionally, involving the school community and parents in these programs enhances their effectiveness.
In a study conducted by XYZ University, it was found that elementary schools that implemented comprehensive prevention programs experienced a significant reduction in the prevalence of childhood obesity compared to schools with minimal or no intervention. The study also highlighted the positive impact of community involvement, parental support, and the role of teachers as role models in promoting healthy behaviors.
Multicomponent Prevention Strategies
School-based obesity prevention programs employ various strategies to create a supportive environment for students to make healthy choices. These strategies revolve around promoting physical activity, encouraging healthy eating habits, and educating students about the importance of maintaining a healthy lifestyle.
The XYZ Elementary School in ABC City is a prime example of a successful school-based program. The school has implemented the following strategies:
- Organizing daily physical education classes to ensure students engage in regular physical activity.
- Offering nutritious meals and snacks in the school cafeteria, with a focus on whole grains, fruits, vegetables, and lean proteins.
- Integrating nutrition education into the curriculum, teaching students about the importance of balanced diets and making healthy food choices.
- Implementing policies that limit the availability of sugary drinks and high-calorie snacks within the school premises.
- Designing a school environment that encourages physical activity, such as providing outdoor play equipment and creating designated spaces for active games.
“Our school has witnessed positive changes in our students’ health and overall well-being since implementing a comprehensive obesity prevention program. By prioritizing physical activity and healthy eating, we are shaping the future health of our students.”
– Jane Smith, Principal of XYZ Elementary School
It is important to note that the long-term implementation of these programs is crucial for sustained benefits. Positive effects may be reversed if the program is discontinued, emphasizing the need for continuous commitment and support from all stakeholders.
Measuring the Success of School-Based Programs
Evaluating the effectiveness of school-based obesity prevention programs is essential for continuous improvement and informed decision-making. By collecting data on key indicators, schools can assess the impact of their interventions and identify areas for further enhancement.
| Evaluation Metrics | Examples |
|---|---|
| Prevalence of childhood obesity | Percentage of students classified as overweight or obese |
| Dietary intake | Consumption of fruits, vegetables, sugary drinks, and unhealthy snacks |
| Physical activity levels | Time spent engaged in moderate-to-vigorous physical activity |
| Knowledge and attitudes | Students’ understanding of healthy eating and the importance of physical activity |
By regularly monitoring these metrics, schools can make data-driven decisions to refine their prevention strategies and allocate resources effectively. Evaluation also provides valuable evidence to support the continuation and expansion of successful programs.
Involving the Community and Parents
A collaborative approach involving the community and parents is essential for the success of school-based obesity prevention programs. When parents are engaged in their child’s health and actively participate in the program, the likelihood of sustained behavior change increases.
The XYZ Elementary School has embraced community involvement by:
- Organizing health fairs and workshops to provide information on healthy eating and physical activity to parents and the community.
- Collaborating with local organizations, such as sports clubs and health clinics, to provide additional resources and support.
- Celebrating student achievements in physical activity and healthy eating through events and awards.
When the school, parents, and the community work together, the impact of prevention strategies is amplified, creating a supportive environment that nurtures healthy behaviors.
In conclusion, school-based obesity prevention programs are vital in promoting healthy behaviors among elementary school students. By implementing comprehensive, multicomponent strategies that combine physical activity with nutrition education and involving the community and parents, schools can significantly reduce the prevalence of childhood obesity and improve overall student well-being.
Effective Strategies in School-Based Obesity Prevention
Implementing effective strategies in school-based obesity prevention programs is crucial for promoting healthy behaviors among children. By addressing various aspects of the school environment and involving key stakeholders, these strategies can have a significant impact on reducing childhood obesity rates.
1. Role of Teachers
Teachers play a vital role in shaping the behaviors and attitudes of students. By acting as role models and actively participating in the delivery of obesity prevention interventions, they can inspire and motivate children to make healthier choices. Teachers should incorporate nutrition education and physical activity into their lesson plans and promote a positive and supportive classroom environment.
2. School Policies
School policies can have a significant influence on students’ food choices and physical activity levels. Implementing policies that support the availability of healthy food choices in school cafeterias and vending machines can encourage students to make nutritious selections. Additionally, limiting the availability of unhealthy snacks and sugary drinks can help reduce excessive calorie intake among students.
Table: Examples of School Policies Supporting Healthy Food Choices
| School Policy | Description |
|———————————————|—————————————————————————————————————–|
| Healthy cafeteria menu | Offering a variety of nutritious food options, such as fruits, vegetables, whole grains, and lean proteins |
| Restricting sugary drinks and snacks | Prohibiting the sale or distribution of sugary drinks and unhealthy snacks within the school premises |
| Nutrition guidelines for school meals | Ensuring that school meals meet specific nutritional guidelines, such as calorie limits and nutrient requirements |
| Promotion of water consumption | Encouraging students to drink water throughout the day and providing easy access to clean drinking water |
3. Parental Involvement
Parents play a crucial role in supporting obesity prevention efforts. Involving parents in the intervention through assignments, meetings, and the dissemination of informative materials can help reinforce healthy habits at home. Schools can provide resources and guidance to parents on creating a healthy home environment, such as tips for meal planning, recipe ideas, and guidelines for limiting screen time.
4. Changes in the School Environment
Creating a supportive school environment is essential for promoting physical activity and reducing sedentary behavior among students. Schools can implement changes such as providing adequate facilities for physical education classes, promoting active transportation (e.g., walking or biking to school), and incorporating movement breaks during classroom time. Additionally, creating safe and engaging outdoor spaces can encourage children to participate in active play.
5. Collaboration with Local Stakeholders
Collaborating with local stakeholders, such as community organizations, health departments, and nonprofit agencies, can enhance the effectiveness of school-based obesity prevention programs. Partnering with these organizations can help schools access additional resources and expertise, share best practices, and promote a coordinated approach to obesity prevention at the community level.
Overall, implementing effective strategies in school-based obesity prevention programs requires a comprehensive approach that involves teachers, school policies, parental involvement, changes in the school environment, and collaboration with local stakeholders. By combining these strategies and promoting a culture of health and wellness in schools, we can make a significant impact on reducing childhood obesity rates and improving the overall health of our children.
Combining Strategies for Effective Obesity Prevention

Combining strategies in obesity prevention programs has proven to be more effective than relying on single strategies alone. By implementing multicomponent interventions that target various environmental and behavioral factors, we can create lasting changes in healthy behaviors and effectively prevent obesity.
One key combination strategy is integrating physical activity with nutrition education. This approach addresses two critical aspects of obesity prevention: promoting regular exercise and emphasizing healthy eating habits. Studies have shown that programs that combine physical activity and nutrition education have achieved statistically significant improvements in obesity-related outcomes.
Furthermore, involving the community and parents in these programs enhances their effectiveness. When local stakeholders, such as schools, community organizations, and parents, actively participate in obesity prevention efforts, it fosters a supportive environment that reinforces healthy behaviors. Community involvement can include organizing health events, providing resources, and spreading awareness about the importance of maintaining a healthy lifestyle.
To illustrate the effectiveness of combining strategies, let’s consider the following data:
| Intervention | Physical Activity | Nutrition Education | Community and Parental Involvement | Outcome |
|---|---|---|---|---|
| Program A | ✓ | ✓ | ✓ | Significant reduction in childhood obesity rates |
| Program B | ✓ | ✓ | x | Moderate reduction in childhood obesity rates |
| Program C | ✓ | x | x | Minimal reduction in childhood obesity rates |
As depicted in the table above, Program A, which combines physical activity, nutrition education, and community and parental involvement, achieves the most significant reduction in childhood obesity rates. This highlights the importance of implementing multicomponent interventions for effective obesity prevention.
In conclusion, combining strategies is vital for the effectiveness of obesity prevention programs. By integrating physical activity, nutrition education, and involving the community and parents, we can create a comprehensive approach that addresses various factors contributing to obesity. These multicomponent interventions have the potential to generate lasting changes in healthy behaviors and mitigate the prevalence of obesity.
Recommendations for Effective School-Based Obesity Prevention

Based on the available evidence, it is recommended that school-based obesity prevention programs adopt a multicomponent approach that combines physical activity, nutrition education, and involvement of the community and parents.
Teachers should play an active role in delivering the intervention and acting as role-models for healthy behaviors.
By actively participating in the intervention, teachers can inspire and motivate students to adopt healthy habits. Through their guidance and support, students can learn the importance of physical activity and nutritious eating, setting the foundation for a lifetime of well-being.
School policies should support the availability of healthy food choices and limit the availability of unhealthy snacks.
By implementing school policies that prioritize nutritious food options and restrict the availability of sugary snacks and beverages, schools can create an environment that encourages and supports healthy eating habits.
Collaboration with local stakeholders and the use of incentives for children can further enhance the effectiveness of these programs.
Engaging local stakeholders, such as healthcare professionals, community organizations, and parents, can provide valuable resources and support for obesity prevention programs. Incentives, such as rewards or recognition for healthy behaviors, can motivate children to actively participate and sustain their engagement in the program.
It is also important to ensure long-term implementation of these programs to sustain the positive effects.
Establishing a long-term commitment to implementing and maintaining obesity prevention programs is crucial in order to see lasting results. Continuous evaluation, monitoring, and adaptation of the programs based on feedback and changing needs are essential for ongoing effectiveness.
Overall, a comprehensive and collaborative approach that involves teachers, schools, parents, and the community is key in effectively preventing obesity among school-aged children.
Recommended Strategies for Effective School-Based Obesity Prevention
To summarize, the following strategies are recommended for effective school-based obesity prevention:
- Adopt a multicomponent approach that combines physical activity and nutrition education.
- Involve teachers as active participants and role-models.
- Implement school policies that support healthy food choices and limit the availability of unhealthy snacks.
- Collaborate with local stakeholders to enhance program effectiveness.
- Utilize incentives to motivate children to actively participate.
- Ensure long-term implementation and evaluation of programs for sustained positive effects.
By following these best practices, schools can make a significant impact in preventing obesity and promoting the health and well-being of their students.
| Strategy | Description |
|---|---|
| Adopt a multicomponent approach | A combination of physical activity and nutrition education is essential for comprehensive obesity prevention. |
| Involve teachers as active participants and role-models | Teachers’ active involvement in delivering the intervention and demonstrating healthy behaviors sets an example for students. |
| Implement school policies supporting healthy food choices | School policies should prioritize nutritious food options and limit access to unhealthy snacks and beverages. |
| Collaborate with local stakeholders | Engaging local healthcare professionals, community organizations, and parents can provide additional support and resources. |
| Utilize incentives to motivate children | Rewards or recognition for healthy behaviors can encourage children to actively participate in the program. |
| Ensure long-term implementation and evaluation | Commitment to sustaining the program and continuously evaluating its effectiveness is crucial for long-term impact. |
Implementing these recommendations and utilizing evidence-based best practices will lead to effective school-based obesity prevention programs that empower students with the knowledge and skills to maintain a healthy lifestyle.
Future Directions in Obesity Prevention

Moving forward, it is crucial to explore innovative approaches and holistic interventions in obesity prevention. The ever-evolving landscape of technology can play a significant role in promoting physical activity and healthy eating habits.
One innovative approach is the incorporation of technology-based interventions, such as mobile apps and wearable devices. These tools can provide individuals with personalized guidance, tracking their activity levels, dietary choices, and even offering real-time feedback and motivational support. By leveraging technology, we can enhance engagement and empower individuals to make sustainable lifestyle changes.
Social media and online platforms also present immense opportunities in obesity prevention. These platforms can be instrumental in reaching larger populations, disseminating evidence-based information, and providing ongoing support. Online communities and forums can foster a sense of belonging and encourage individuals to share their experiences, challenges, and successes, creating a supportive network that inspires and motivates.
Addressing the underlying social and environmental determinants of obesity is crucial for long-term success. By understanding and addressing socioeconomic factors, such as access to affordable healthy food options and opportunities for physical activity, we can create environments that enable healthier choices. Collaborating with stakeholders from diverse sectors, including policymakers, urban planners, and healthcare providers, is instrumental in shaping policies and initiatives that promote a healthier society.
As we continue our efforts in obesity prevention, it is essential to embrace a holistic approach that encompasses various facets of an individual’s life. This includes education, community engagement, policy changes, and addressing social determinants that influence health outcomes. By adopting innovative approaches and implementing comprehensive interventions, we can make significant progress in preventing obesity and improving public health.
Conclusion
Obesity prevention requires a population-based and multilevel approach that focuses on environmental and policy change and involves participation from multiple sectors. By implementing effective strategies in school-based obesity prevention, such as combining physical activity with nutrition education, involving teachers, parents, and the community, and implementing supportive school policies, we can make significant progress in reducing the prevalence of obesity.
For successful implementation of these programs, long-term commitment is crucial. Collaboration with local stakeholders and the incorporation of innovative approaches, such as technology-based interventions, can enhance the effectiveness of obesity prevention measures. Future directions in obesity prevention should explore holistic interventions that address the underlying social and environmental determinants of obesity.
By continuously evaluating and adapting programs based on evidence-based strategies and best practices, we can work towards improving public health and creating a healthier future for generations to come.




